People’s minds are pretty well made up when it comes to boosters for Covid 19. It’s hard to change anyone’s opinion regarding their safety or effectiveness. Sad. Here is a summary of some modelling about the number of lives and dollars that could be saved with two different vaccination rate scenarios.
Leading the NewsAnalysis suggests nearly 90K deaths could be prevented this fall and winter by greater uptake in COVID-19 boostersCNN (10/5, Howard) reports, “COVID-19 vaccinations could save thousands of lives and billions of dollars this winter.” An analysis by The Commonwealth Fund found that “if 80% of eligible people receive their booster dose…it would prevent about 90,000 deaths and more than 936,000 hospitalizations and prevent $56 billion in medical costs in the next six months compared with the baseline scenario.” But, “if booster vaccinations remain at their current pace, the researchers found, a potential COVID-19 winter surge could bring a peak of about 16,000 hospitalizations and 1,200 deaths per day by March.” |
Here is the original article:
A Fall COVID-19 Booster Campaign Could Save Thousands of Lives, Billions of Dollars
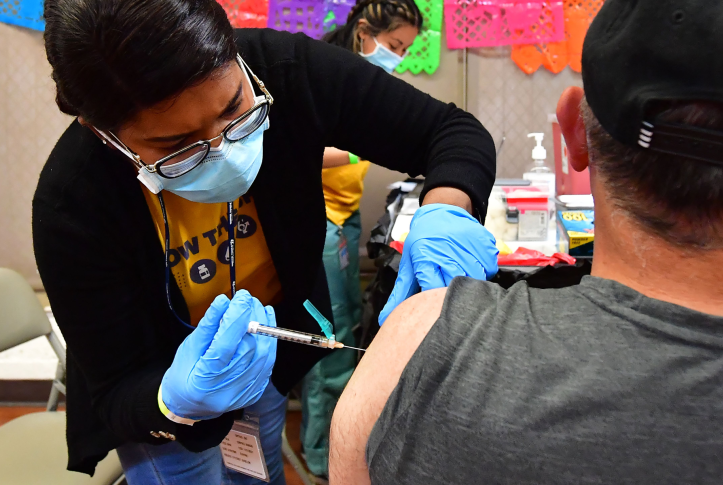
Registered nurse Mariam Salaam administers a booster shot at a COVID vaccination and testing site in Los Angeles on May 5, 2022. A fall booster vaccination campaign could drastically reduce deaths and hospitalizations this winter. Photo: Frederic J. Brown/AFP via Getty Images
-
Faculty, Center for Vaccine Development and Global Health, University of Maryland
-
Senior Research Associate, Policy and Research, The Commonwealth Fund
-
Professor of Applied Mathematics and Computational Epidemiology, York University
-
Postdoctoral Researcher, York University
-
Research Scientist in Epidemiology (Microbial Diseases), Yale School of Public Health
-
Founding Director, Yale Center for Infectious Disease Modeling and Analysis (CIDMA); Burnett and Stender Families Professor of Epidemiology, Yale School of Public Health
-
With COVID-19 booster uptake low and federal funding for vaccination campaigns drying up, new bivalent boosters may not achieve high enough coverage to curb the predicted surge in cases this winter
-
A Commonwealth Fund study finds federal investment in vaccination campaigns could prevent thousands of hospitalizations and deaths and generate billions in savings
COVID-19 vaccination has substantially mitigated the burden of COVID-19, preventing millions of deaths and hospitalizations since the first vaccines were rolled out in late 2020. As of early September 2022, updated bivalent boosters, or boosters that provide protection against both the original virus strain as well as the Omicron variant (and its subvariants like BA.4 and BA.5), have been authorized. These are available for anyone who has completed their primary vaccination series and has not received any additional doses for at least two months.
Boosters are a necessary part of COVID-19 mitigation because vaccine-induced and natural protection against disease have been shown to be transient. However, booster uptake in the United States has steadily declined since the initial wave of the Omicron variant, and federal financial support for vaccination campaigns has not been replenished, partly because of the perception that the pandemic is over. As of October 3, 68 percent of the total U.S. population has been vaccinated with a primary series, but fewer than half of fully vaccinated individuals have received a booster dose. Only 36 percent of people age 50 and older have received their second booster dose. The rates of vaccination, including boosters, declined to less than 100,000 doses administered daily by September 12. That number is beginning to increase as more people get updated booster shots, but dwindling federal funding for vaccination threatens to undermine any goal of high coverage.
In this post we update our analysis from July and examine the potential impact of a surge in cases during the upcoming fall and winter. We evaluated the impact of accelerated delivery of booster doses on reducing hospitalizations, deaths, and direct medical costs. We conducted this analysis using a previously developed simulation model to estimate the impact of vaccination rates under different scenarios. To inform congressional decisions about federal spending, we identified the cost savings that would specifically accrue to the Medicare and Medicaid programs and compared these savings to anticipated expenditures on accelerated vaccination campaigns. (See “How We Conducted This Study” for further details.)
We examined three scenarios: a baseline scenario where daily vaccination rates remain unchanged and two vaccine campaign scenarios in which rates increased by the end of 2022. For the baseline scenario, we assumed that from September 2022, vaccination will continue at the same rate as the average in August (i.e., about 28 vaccine doses per 100,000 population per day) until the end of March 2023. In the two vaccine campaign scenarios, we simulated two different fall vaccination campaigns delivering booster doses to individuals age 5 and older at increased rates between October 1 and December 31, and at baseline rates for other times. (Following the operational guidelines of the Centers for Disease Control and Prevention (CDC) and in light of the Pfizer application regarding pediatric boosters, we considered those age 5 and older to be eligible if they had received the last dose of their primary series or booster dose at least four months prior.)
The two vaccine campaign scenarios where rates increase differ in the level of coverage achieved:
- In the first scenario, we estimated COVID booster uptake for the eligible population based on age-specific influenza vaccination coverage in 2020–2021 by the end of 2022
- In the second, we assume 80 percent of eligible individuals age 5 and older receive their booster dose by the end of 2022.
We then determined the estimated impact of these potential campaigns by comparing the projected number of infections, hospitalizations, deaths, and direct medical costs from October 1 to March 31 to the baseline scenario. For this analysis, we stratified estimates of cost savings by payer (e.g., Medicare, Medicaid, commercial insurance companies).
We estimated a fall booster vaccination campaign that reaches coverage similar to the 2020–2021 influenza vaccination (scenario 1) would prevent more than 75,000 deaths and more than 745,000 hospitalizations and generate savings of $44 billion associated with direct medical costs by the end of March 2023, compared to the baseline. An even more successful campaign (scenario 2) would prevent approximately 90,000 deaths, more than 936,000 hospitalizations, and avert $56 billion in direct medical costs over the course of the next six months, compared with the baseline scenario.
If vaccination continued at its current pace through the end of March 2023, a potential winter surge in COVID-19 infections could result in a peak of around 16,000 hospitalizations and 1,200 deaths per day by March 2023. Under both scenarios modeled, we found an aggressive fall booster vaccination campaign could prevent COVID-19 deaths from exceeding 400 per day.
In addition to preventing illness and death, accelerated vaccination campaigns would save money. Stratifying by insurance type, we found direct medical costs would be reduced by $11 billion for Medicare alone under scenario 1 and $13 billion under scenario 2. An additional $3.5 to $4.5 billion in savings would accrue to Medicaid. Even if the federal government paid all vaccination costs, accelerated campaigns would generate more than $10 billion in net savings from federal programs like Medicare and Medicaid.
An Effective Booster Campaign Needs Ongoing Vaccination Funding
As population immunity wanes and new variants capable of evading protection from earlier vaccines and natural infection continue to emerge, surges in hospitalizations and deaths during the upcoming fall and winter are increasingly likely. Federal funding for COVID-19 vaccines and treatments has stagnated, hindering access at a crucial time. The recent FDA approval of bivalent boosters offers an opportunity to curb transmission; a vaccination campaign that moves aggressively could avert a surge of hospitalizations and deaths, and save money in the process.
We adapted our age-stratified, agent-based model of COVID-19 to account for the waning of naturally acquired or vaccine-elicited immunity. The model was calibrated by fitting to the reported variant-specific incidence of COVID-19 between October 2020 and August 31, 2022. The fitted model was validated using the trends of hospitalizations and deaths during the same period. We then simulated our model forward from September 1, 2022, to March 31, 2023, under a baseline and counterfactual scenarios of booster vaccination campaigns. In the baseline scenario, the daily rate of vaccination was set to the average daily number of 28 vaccine doses per 100,000 population administered during August 2022 and continued until March 31, 2023. In counterfactual scenarios, this average rate was maintained through September 30, 2022, before initiation of accelerated fall vaccination campaigns.
Accelerated vaccination campaigns were implemented between October 1 and December 31, 2022. We considered two campaign scenarios that differed in the coverage achieved. In the first scenario we implemented age-specific rates of vaccination, such that age-specific booster coverage among the eligible population would be the same as vaccination coverage achieved for the 2020–2021 influenza season. Under a second, more ambitious scenario, we considered an 80 percent booster coverage of eligible individuals age 5 and older. Following the operational guidelines (as of August 20, 2022) of the Centers for Disease Control and Prevention (CDC), and in light of the Pfizer application regarding pediatric bivalent boosters, we considered those age 5 and older to be eligible if they had received the last dose of their primary series or booster dose at least four months prior. We projected the number of infections, hospitalizations, and deaths between October 1, 2022, and March 31, 2023, for the baseline scenario and each counterfactual.
Although the bivalent vaccines have been shown to generate significantly higher levels of neutralizing antibodies against the Omicron subvariants, real-world estimates of their effectiveness are currently lacking. In our analysis, we conservatively set the effectiveness of the bivalent vaccines against infection, symptomatic infection, and severe disease caused by the BA.4 and BA.5 subvariants to those observed for a booster dose of the monovalent vaccines countering the BA.1 subvariant.
We calculated the direct medical cost savings generated as a result of accelerated vaccination campaigns compared to the baseline by multiplying the total number of averted symptomatic cases, severe nonhospitalized cases, hospitalized cases, and ICU cases by their average unit cost. Our analyses conservatively include only direct medical costs, although indirect costs and productivity losses also would be substantial. Costs vary according to symptom severity. Specifically, a proportion of mildly symptomatic individuals incur outpatient cost. Inpatient cost for symptomatic individuals requiring hospitalization varied based on whether they were admitted to an intensive care unit (ICU), for which we used hospitalization with or without ventilation as a proxy for cost of ICU or non-ICU, respectively. Transportation cost for each inpatient hospitalization was estimated by multiplying the average cost per round-trip to a health care facility with an average number of 2.5 emergency medical services (EMS) calls per inpatient. We assumed that symptomatic individuals with severe infection who are not hospitalized required one emergency department visit on average.
We stratified cost savings by the insurance category to which the savings would accrue, including Medicare, Medicaid, private health insurance, and the uninsured. We first applied the age-specific insurance coverage by each insurance type to the age-specific health outcomes, and then multiplied these insurance-stratified outcomes by insurance-specific unit costs. Insurance-specific costs were not available for emergency department visits or EMS calls, so these were kept constant across all payers.
The cost of one vaccine dose was set to the list price of $19.50 per dose for the Pfizer-BioNTech vaccines, which is the higher price of the two approved mRNA vaccines. The administration fee was set to the current Medicare reimbursement payment of $40.
Note on Estimates
Our results conservatively estimate vaccination impact in three aspects:
First, SARS-CoV-2 mutates rapidly, with immune-evasive variants continuously challenging control. Since we did not consider the rise of yet another immune-evasive variant in our analysis, the estimated magnitude of the surge is primarily driven by waning immunity. With the rise of new Omicron subvariants, or an entirely new variant, the surge could be significantly larger, and our results may therefore underestimate the benefits of bivalent booster vaccination in terms of cases, hospitalizations, deaths, and medical costs averted.
Second, CDC has recently updated guidance regarding isolation of individuals with COVID-19 and quarantine of those who have been exposed. However, as we do not yet have concrete data regarding adherence to previous guidance or behavioral changes in the wake of the update, we did not include this element in our projections. These relaxed measures are likely to fuel a more substantial fall surge than predicted here, as many people remain infectious beyond the fifth day following symptom onset, and their increased circulation in the community contributes to onward transmission.
Third, we did not incorporate holiday-driven contact into our simulations. Many people celebrated fall and winter holidays modestly in 2020 and 2021, but this may not hold true for 2022, which could similarly drive a higher, earlier peak in COVID-19 cases than projected by our model. Finally, we did not include the costs associated with long COVID. The health and economic benefits from preventing these outcomes would be considerable.




