Covid 19 cases are declining, but not rapidly. The speed at which the slope declines depends on how much virus is circulating. Hopefully, by Halloween, there will be approval for children to be vaccinated. In the meantime, mask wearing reduces the risk of spread in adults as well as children. There is someone on our street who has a sign in their yard saying “Unmask our kids.” Every parent wants to keep their children safe. Here are two studies which show that there is a simple and safe way to do it.
CNN)Covid-19 outbreaks are far more likely in schools that don’t require students and staff to wear masks, new data from the US Centers for Disease Control and Prevention shows.
Two studies released Friday support the agency’s recommendation for universal indoor masking in schools.
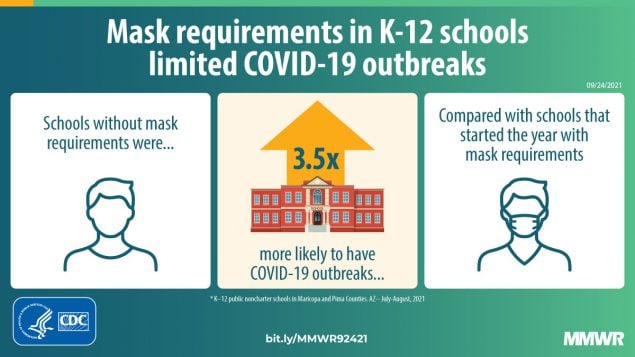
One study in Arizona showed schools with no masking requirement were about 3.5 times more likely to have a Covid-19 outbreak than schools that had a universal masking requirement.
A second study showed counties across the US where schools required mask use also had less transmission of the virus in the community in general.
For the first study, researcher looked at data covering about 1,000 K-12 schools in Arizona’s Maricopa and Pima Counties, which are home to more than three-quarters of the state’s population.
A school was considered to have a masking requirement if all people — including students, staff, faculty and visitors — were required to wear a mask indoors, regardless of vaccination status. A school was considered to have an outbreak if there were two or more news cases among students or staff within a 14-day period, beginning a week after school started.
From mid-July through the end of August, 191 school-associated outbreaks occurred, according to the CDC. Schools with universal masking requirements in place at the start of school accounted for about 31% of the set of schools analyzed, but only about 8% of outbreaks. Meanwhile, schools with no masking requirement accounted for 59% of those outbreaks, but less than half (48%) of the total set of schools analyzed.
In early August, the CDC adjusted recommendations for masking in schools to include everyone, regardless of vaccination status, due to the prevalence of the more contagious Delta variant.
“I would say that data actually absolutely show that masking decreases outbreaks in schools,” CDC Director Dr. Rochelle Walensky said Monday. “So with the purpose of keeping our kids in school, getting them in school, having them be safe, masks really are the way to go.”
Another CDC study published Friday suggests that the effects of masking policies in schools appear to extend beyond classroom walls, too.
The study found that case rates among children increased more in counties where schools did not have mask requirements than they did in counties where schools mandated universal masking.
Here are the studies:
Pediatric COVID-19 Cases in Counties With and Without School Mask Requirements — United States, July 1–September 4, 2021
Early Release / September 24, 2021 / 70
Samantha E. Budzyn, MPH1,2; Mark J. Panaggio, PhD3; Sharyn E. Parks, PhD1; Marc Papazian4; Jake Magid; M Eng4; Lisa C. Barrios, DrPH1 (View author affiliations)
Consistent and correct mask use is a critical strategy for preventing the transmission of SARS-CoV-2, the virus that causes COVID-19 (1). CDC recommends that schools require universal indoor mask use for students, staff members, and others in kindergarten through grade 12 (K–12) school settings (2). As U.S. schools opened for the 2021–22 school year in the midst of increasing community spread of COVID-19, some states, counties, and school districts implemented mask requirements in schools. To assess the impact of masking in schools on COVID-19 incidence among K–12 students across the United States, CDC assessed differences between county-level pediatric COVID-19 case rates in schools with and without school mask requirements.
Using data from July 1–September 4, 2021, counties that met the following criteria were included in the analysis: 1) a valid school start date, and MCH Strategic Data* included a known school mask requirement for at least one district; 2) in districts with known school mask requirements, a uniform mask requirement for all students or no students; and 3) at least 3 weeks with 7 full days of case data since the start of the 2021–22 school year. For counties with multiple school districts, the median school start date was used. Counties with conflicting school mask requirements were excluded from this analysis; only those counties with the same known mask requirements for all schools were included. Among the 3,142 U.S. counties included in the initial sample, 16.5% (520) were included in the final analysis after applying the selection criteria. County-specific pediatric COVID-19 rates (number of cases per 100,000 population aged <18 years) from CDC’s COVID Data Tracker† were tabulated and aggregated by school start week. To account for the variation in the weeks each county started school, weeks were numbered from −3 to 2; the school start date was the beginning of week 0. Aggregated pediatric COVID-19 case counts and rates were calculated; average weekly changes were compared for counties with and without school mask requirements using a one-sided t-test. To further assess the association between pediatric COVID-19 cases and school mask requirements, a multiple linear regression was constructed that adjusted for age, race and ethnicity,§ pediatric COVID-19 vaccination rate, COVID-19 community transmission, population density, social vulnerability index score,¶ COVID-19 community vulnerability index score,** percentage uninsured, and percentage living in poverty. Statistical analyses were completed using SciPY (version 1.2.1) and Statsmodels (version 0.11) analysis modules for Python (version 3.7.6; Python Software Foundation). Statistical significance was defined as p<0.05 for all analyses. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.††
Counties without school mask requirements experienced larger increases in pediatric COVID-19 case rates after the start of school compared with counties that had school mask requirements (p<0.001) (Figure). The average change from week −1 (1–7 days before the start of school) to week 1 (7–13 days after the start of school) for counties with school mask requirements (16.32 cases per 100,000 children and adolescents aged <18 years per day) was 18.53 cases per 100,000 per day lower than the average change for counties without school mask requirements (34.85 per 100,000 per day) (p<0.001). Comparisons between pediatric COVID-19 case rates during the weeks before (weeks −3, −2, and −1) and after (weeks 0, 1, and 2) the start of school indicate that counties without school mask requirements experienced larger increases than those with school mask requirements (p<0.05). After controlling for covariates, school mask requirements remained associated with lower daily case rates of pediatric COVID-19 (β = −1.31; 95% confidence interval = −1.51 to −1.11) (p<0.001).
The findings in this report are subject to at least four limitations. First, this was an ecologic study, and causation cannot be inferred. Second, pediatric COVID-19 case counts and rates included all cases in children and adolescents aged <18 years; later analyses will focus on cases in school-age children and adolescents. Third, county-level teacher vaccination rate and school testing data were not controlled for in the analyses; later analyses will control for these covariates. Finally, because of the small sample size of counties selected for the analysis, the findings might not be generalizable.
The results of this analysis indicate that increases in pediatric COVID-19 case rates during the start of the 2021–22 school year were smaller in U.S. counties with school mask requirements than in those without school mask requirements. School mask requirements, in combination with other prevention strategies, including COVID-19 vaccination, are critical to reduce the spread of COVID-19 in schools (2).
Association Between K–12 School Mask Policies and School-Associated COVID-19 Outbreaks — Maricopa and Pima Counties, Arizona, July–August 2021
Early Release / September 24, 2021 / 70
Megan Jehn, PhD1,*; J. Mac McCullough, PhD2,*; Ariella P. Dale, PhD3,4; Matthew Gue1; Brian Eller5; Theresa Cullen, MD5; Sarah E. Scott, MD4 (View author affiliations)
CDC recommends universal indoor masking by students, staff members, faculty, and visitors in kindergarten through grade 12 (K–12) schools, regardless of vaccination status, to reduce transmission of SARS-CoV-2, the virus that causes COVID-19 (1). Schools in Maricopa and Pima Counties, which account for >75% of Arizona’s population (2), resumed in-person learning for the 2021–22 academic year during late July through early August 2021. In mid-July, county-wide 7-day case rates were 161 and 105 per 100,000 persons in Maricopa and Pima Counties, respectively, and 47.6% of Maricopa County residents and 59.2% of Pima County residents had received at least 1 dose of a COVID-19 vaccine. School districts in both counties implemented variable mask policies at the start of the 2021–22 academic year (Table). The association between school mask policies and school-associated COVID-19 outbreaks in K–12 public noncharter schools open for in-person learning in Maricopa and Pima Counties during July 15–August 31, 2021, was evaluated.
A school was considered to have a mask requirement if all persons, regardless of vaccination status, were required to wear a mask indoors in school. An early mask requirement was one that was in place when the school year began, and a late mask requirement was one that was implemented any time after school began. Mask policies were abstracted from publicly available school COVID-19 mitigation plans, which must be posted online per Executive Order 2020–51.† A school-associated outbreak was defined as the occurrence of two or more laboratory-confirmed COVID-19 cases§ among students or staff members at the school within a 14-day period and at least 7 calendar days after school started, and that was otherwise consistent with the Council for State and Territorial Epidemiologists 2020 outbreak definition¶ and Arizona’s school-associated outbreak definition.** In Arizona, school-associated outbreaks are required to be reported to the local public health agency within 24 hours; data are stored in Arizona’s Medical Electronic Disease Surveillance Intelligence System. School characteristics, including county of location, grade levels present,†† enrollment, and Title I status§§ (a measure of a school population’s socioeconomic status) were obtained from the Arizona Department of Education. Crude and adjusted logistic regression analyses with 95% confidence intervals (CIs) were performed in Stata (version 15; StataCorp) and adjusted for school county, enrollment size, grade levels present, Title I status, and 7-day COVID-19 case rate in the school’s zip code during the week school commenced. Schools with late mask requirements were excluded from these analyses because of their mixed exposure status during the sampling time frame (e.g., schools might have enacted mask requirements after an outbreak). Vaccination coverage for staff members and students was not available at the school level.
Data were available for 1,020 of 1,041 (98.0%) K–12 public noncharter schools in Maricopa and Pima counties. Twenty-one (2.0%) schools had outbreaks reported <7 days after school began and were excluded from the analyses. Among the 999 (96.0%) schools included in the analysis, 210 (21.0%) had an early mask requirement, 309 (30.9%) had a late mask requirement enacted a median of 15 days after school started (interquartile range = 9–17 days), and 480 (48.0%) had no mask requirement (Table). During July 15–August 31, 2021, 191 school-associated outbreaks occurred, 16 (8.4%) in schools with early mask requirements, 62 (32.5%) in schools with late mask requirements, and 113 (59.2%) in schools without a mask requirement.
In the crude analysis, the odds of a school-associated COVID-19 outbreak in schools with no mask requirement were 3.7 times higher than those in schools with an early mask requirement (odds ratio [OR] = 3.7; 95% CI = 2.2–6.5). After adjusting for potential described confounders, the odds of a school-associated COVID-19 outbreak in schools without a mask requirement were 3.5 times higher than those in schools with an early mask requirement (OR = 3.5; 95% CI = 1.8–6.9).
CDC recommends universal indoor masking in K–12 schools (1); however, masking requirements in K–12 schools vary by school district, county, and state. In the two largest Arizona counties, with variable K–12 school masking policies at the onset of the 2021–22 academic year, the odds of a school-associated COVID-19 outbreak were 3.5 times higher in schools with no mask requirement than in those with a mask requirement implemented at the time school started. Lapses in universal masking contribute to COVID-19 outbreaks in school settings (3); CDC K–12 school guidance recommends multiple prevention strategies. Given the high transmissibility of the SARS-CoV-2 B.1.617.2 (Delta) variant, universal masking, in addition to vaccination of all eligible students, staff members, and faculty and implementation of other prevention measures, remains essential to COVID-19 prevention in K–12 settings (1).
Acknowledgments
Angelica Flores; Raymond Gue; Matthew Speer; Va’Trelle Stokely; Jessica Wani; Carly Whalen; Parker Young; Jennifer Collins; Christina Mrukowicz; Brandon Howard; Kasey Busick; Matthew Christenberry; Amanda Sapp; Maricopa County Department of Public Health Cluster Response Team; Arizona Department of Education; Maricopa County and Pima County K–12 school partners.




