The FDA cancelled their meeting today to discuss next year’s flu vaccine. No explanation given. This is very disturbing as it was announced that this is the worst flu season in 15 years. Here is some data from infectious disease specialist Dr. Paul Sax’s blogpost. Also official, the first case of measles in the San Antonio was reported in in a charter school in the Cibolo area. This is very disturbing given this disease had been eradicated in this country in 2000.
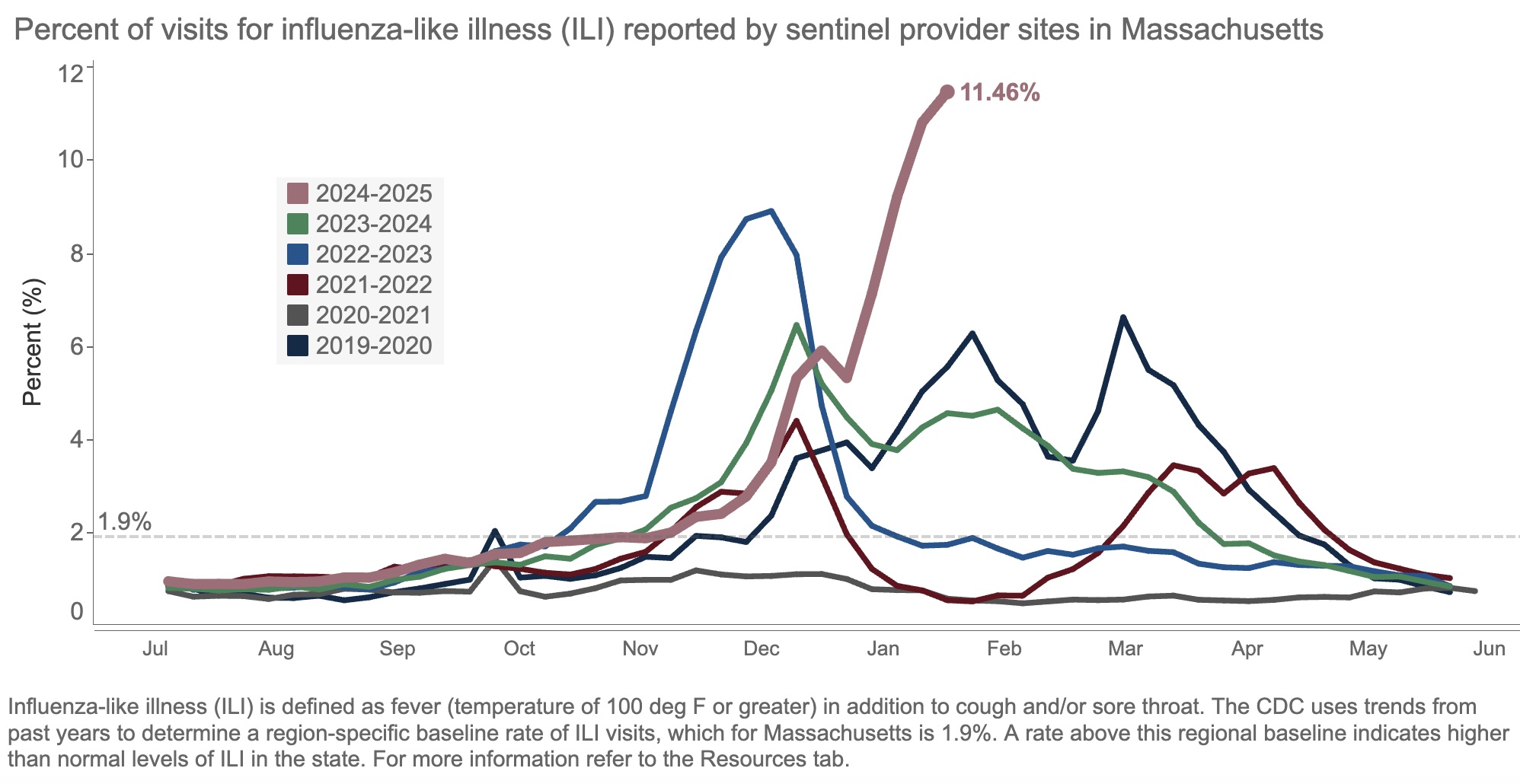
The result of all this “influenza-like illness”? Patients are deluging outpatient clinicians with messages about fevers, sore throats, coughs, and related symptoms. Hospital beds and ICUs fill up with chronically ill people whose condition has worsened due to the flu. Emergency rooms, already overstrained, park sick people in hallways awaiting evaluation and treatment.
Yes, it’s bad out there, folks. This week, we heard that our hospital has four times as many people hospitalized with the flu than as those hospitalized with COVID-19, the first time this has happened since the pandemic.
One of the most common questions we ID doctors get when the flu season is bad, or late, or just strange, is, “Why this year?” The honest answer is this humble three-word sentence:
We don’t know.
Some have blamed the cold weather this winter without much in the way of a significant thaw. Maybe, but other cold winters haven’t necessarily had this much flu. Plus there’s plenty in southern states.
Others cite the low rate of influenza vaccination, in reaction to overzealous (in some views) COVID-19 vaccine recommendations. Perhaps, but this has never been a popular vaccine.
A third theory is the fact that masking and other infection prevention activities in the community have ended. I doubt it’s this because masking was pretty much over last year and even the year before.
Some have asked me if this year’s strain of flu is somehow different, and the answer is that surveillance molecular data do not so far suggest this is the case. This is in contrast to the 2009 H1N1 influenza pandemic, where during April (!) flu cases surged because of the emergence of a novel H1N1 variant to which younger people had little immunity.
Related, one cause of this year’s high number of cases emphatically isn’t a flood of cases of “highly pathogenic” avian influenza, H5N1. Despite active surveillance at the state level, we still are not seeing this illness from this strain to a significant degree — fortunately!
Note that I put the words “highly pathogenic” in quotes. H5N1 is of course of great concern because we have no natural immunity to it. If it emerges as a human-to-human pathogen, we’re looking at an explosion of cases, analogous to or worse than 2009. That’s bad enough.
But another major worry is that it might be intrinsically more virulent, more likely to cause severe disease per case. But the cases of H5N1 reported thus far in the United States from animal sources have had a wide spectrum of severity. At one extreme there has been a death, and at least one ICU admission; at the other end of the spectrum, many have had mild illness (conjunctivitis seems particularly common), and a recent serologic study in 150 bovine veterinary practitioners found 3 positive cases — all asymptomatic.




