4 New Things About Covid-19:
1. There is more of it. What follows is a report from the Methodist Health Care System which confirms what I knew from the phone calls that I have been getting for the last 10 days. Covid-19 cases have risen dramatically. The increase had been in the 20-30-year-old age range, but the range of ages of those hospitalized ranges from 35-89 according to one infectious disease specialist. This is tragic, because it is so preventable.
“Methodist Healthcare has 83 known COVID-19 positive patients under our care. Over the past week, we have experienced a significant increase in the number of COVID patients. The number of hospitalized patients in MHS hospitals has risen from 29 patients on June 1 and 37 patients on June 10. Patients hospitalized within all San Antonio hospitals with COVID infection has increased from 93 on June 1 and 108 on June 10 to 241 today. We have seen an increase in the proportion of our hospitalized patients in the 20-34 and 35-54 age groups. ”
2. Chloroquine is out per the FDA. There was a lot of controversy regarding the most recent article on it from the British journal, Lancet, but the FDA felt there was enough data in other studies to rescind its approval for the treatment of Covid-19. FDA on hydroxychloroquine/chloroquine: The FDA has revoked its emergency use authorization for hydroxychloroquine and chloroquine as COVID-19 treatments. The agency says that the drugs are “unlikely to be effective in treating COVID-19. … Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.” Emergency use authorization was initially granted for the drugs on March 28.”
3. Earlier studies showed that high dose of steroids was associated with increased mortality in patients severely ill with Covid-19. This is a randomized-controlled study which has yet to be published in a peer-reviewed journal, but which shows that low dose dexamethasone may be effective in reducing mortality. Low-dose dexamethasone: Dexamethasone is associated with reduced mortality risk among patients with severe COVID-19, making it the first drug to show such an effect, according to a statement by trial investigators at the University of Oxford. Over 6000 hospitalized patients were randomized to receive either dexamethasone (6 mg daily) or usual care for 10 days. Dexamethasone was associated with significantly lower risk for death among ventilated patients (rate ratio, 0.65) and other patients receiving oxygen (RR, 0.80), compared with those given usual care. Patients who didn’t require respiratory support did not see a benefit. The authors estimate that eight ventilated patients or 25 patients requiring only oxygen would need to be treated with dexamethasone to prevent one death. The results have not been published in a journal yet. The bottom line is this isn’t something for outpatient treatment.
Here are the University of Washington Guidelines regarding steroids:
Steroids: There is no clinical evidence of net benefit from steroids in SARS-CoV, MERS-CoV or influenza infection, and observational data show increased mortality, more secondary infections, impaired viral clearance and more adverse effects in survivors Effects of early corticosteroid treatment on plasma SARS-associated Coronavirus RNA concentrations in adult patients; Clinical management of severe acute respiratory infection when novel coronavirus (nCoV) infection is suspected. However, a new retrospective cohort (201 patients, 84 [42%] of whom developed ARDS) demonstrated that among patients with ARDS, methylprednisolone decreased risk of death (HR, 0.38; 95% CI, 0.20-0.72) Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. May use corticosteroids if required for other indications and use the lowest dose for the shortest duration.
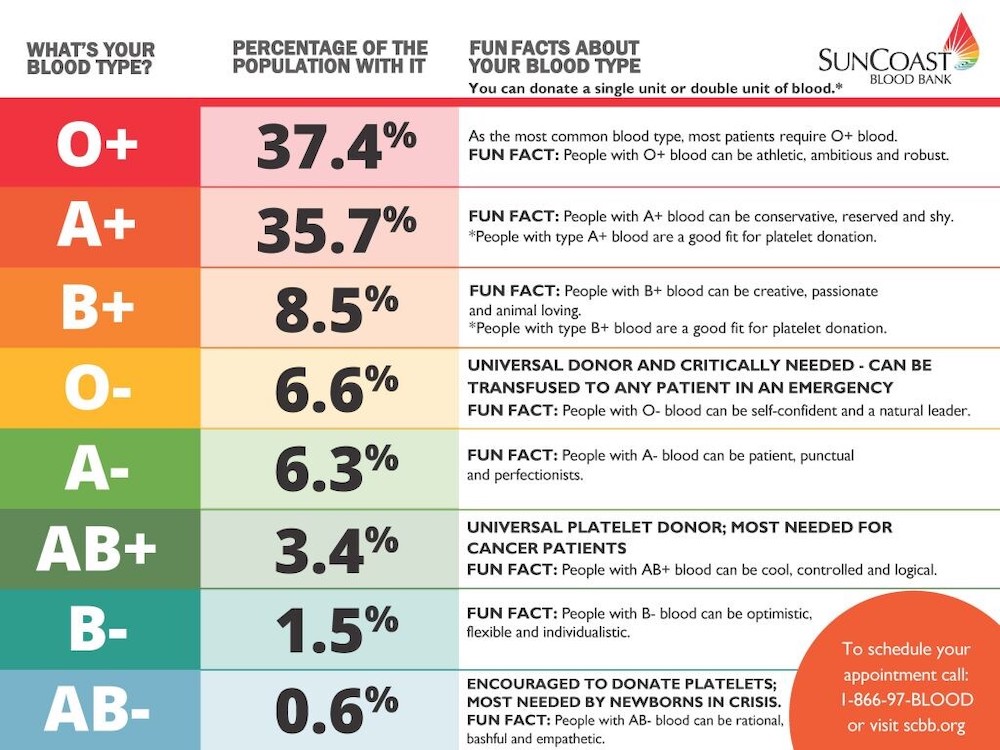
4. Genetic differences may explain different clinical courses. Why do some people have minimal illness and other people dies from Covid-19? Genetic differences may play a part as suggested in the new study in the New England Journal of Medicine which showed that patients in Italy and Spain with different blood types(which are genetically determined) were associated with different outcomes. Note that this is not proof of cause and effect, does give guidance to people with different blood types and has no therapeutic consequence.
Blood type and risk: A genome-wide association study in the New England Journal of Medicine finds that patients with blood type A are at increased risk for COVID-19-induced respiratory failure than other blood groups. Researchers compared the genomes of roughly 1600 people with severe COVID-19 in Italy and Spain with over 2200 uninfected population-based controls. Two chromosomal loci were associated with COVID-19-induced respiratory failure. One of these is also the ABO blood group locus. Blood group A was associated with a 45% increased risk for COVID-19 respiratory failure, while blood group O was associated with a 35% lower risk, relative to other blood groups. The other affected locus covered genes that have functions that could be relevant to severe COVID-19, such as interacting with the SARS-CoV-2 cell-surface receptor.
The most common blood types?