HOT WEATHER POSTS
COVID FATIGUE
FALL VACCINE UPDATE
RSV VACCINE GUIDELINES
FLU VACCINE
MEDICARE ADVANTAGE
Kids may have gone back to school, but summer is by no means over. I have posted some usual summer topics on my blog which deal with things like preventing heat injury, sunburn prevention and avoiding mosquitoes. On the last note, two mosquitoes in Bexar County were recently identified as carrying West Nile Virus. That is something I am anxious to avoid. Here are some links to those topics if you are interested. I also threw in a New England Journal of Medicine article analyzing the pros and cons of different diets.
Insect Repellants and Sunscreens Revisited – Mark Thornton (personalphysicianmd.com)
Avoiding Heat Stroke – Mark Thornton (personalphysicianmd.com)
Diets: A Review Article from NEJM – Mark Thornton (personalphysicianmd.com)
Covid Fatigue
We have it. Never have we seen so many cases. One day we had 10 cases, a clinic record. Most of these are diagnosed with home tests. Three patients required hospitalization. Mild cases may just be treated with medications that would normally be used for colds, but more severe cases and/or those in people with increased risk of severe Covid are treated with Paxlovid. Do I Need Paxlovid? – Mark Thornton (personalphysicianmd.com).
The virus now seems to peak twice a year in the summer and winter. A new vaccine based on the JN1 subvariant, KP.2, should be available in the coming weeks. The most recent strains KP.1,2 and 3( KP3.1.1 is now the dominant variant in the US) are different enough that previous infections and immunizations are not going to be enough to protect you. Getting a Covid vaccine can reduce your risk of getting the virus by 50% and reduce your risk of getting Long Covid by 26%. Some people have concerns about the vaccines. I’m getting it. Incidentally, a recently released study did confirm what we had previously suspected that people who had more side effect such as fever, body aches and malaise, had more pronounced antibody responses to the vaccine.
Map shows states where COVID levels are “high” or “very high” as summer wave spreads
More than half of states are now seeing “high” or “very high” levels of SARS-CoV-2, the virus that causes COVID-19, in their wastewater testing, according to figures published Friday by the Centers for Disease Control and Prevention, as this summer’s COVID wave reaches a growing share of the country.
Nationwide, the CDC now says that the overall level of SARS-CoV-2 in wastewater is “high” for the first time since this past winter. Levels remain “high” across western states, where trends first began to worsen last month, while other regions are now seeing steeper increases at or near “high” levels.
Friday’s update is the first since last month, due to the Fourth of July holiday.
The uptick is in line with a growing number of COVID-19 patients showing up in emergency rooms. The District of Columbia and 26 states are now seeing “substantial increases” in COVID-19 emergency room visits, the agency says.
Nationwide, the average share of emergency room patients with COVID-19 is also now the highest it has been since February and has increased 115% from a month ago.
Overall emergency room visits and hospitalization trends remain at what the CDC deems to be “low” levels in several states, far below the deadly peaks reached at earlier points during the pandemic.
But COVID-19 emergency room visits crossed the threshold into “moderate” levels in Hawaii last month, after a surge that topped the last two waves of the virus. Florida also is now at “moderate” levels, amid a wave that is at peaks not seen since this past winter.
“We are seeing patterns that are consistent with what we have observed over the last couple of years in the summer, where we have seen upticks in activity that have occurred around this time of year that are not quite as large as what we see during the winter peaks,” said Aron Hall, deputy director for science in the CDC’s Coronavirus and Other Respiratory Viruses Division.
Health authorities in some communities have said in recent weeks that the uptick is a sign that now could be the time for people looking to avoid COVID-19 infections — especially at-risk Americans, with underlying health issues — to start taking extra precautions like masking and testing in many parts of the country.
Hall said the recent increase did not look to be any more severe than previous summer waves, but served as a reminder of the importance of getting vaccinated and other steps, like seeking out treatment for those at increased risk of severe disease.
“The activity that we are seeing now is consistent with previous trends. It is not necessarily cause for any additional alarm, but is an important reminder that there are key measures that folks can take to protect themselves,” he said.
When will COVID-19 peak this summer?
Most of the first states to reach “high” COVID-19 levels in wastewater last month were in the West, where the share of COVID-19 patients in emergency rooms has also accelerated. Reported infections in nursing homes have also grown in this region.
Other countries have also seen COVID-19 trends rise this summer earlier than last year. In the United Kingdom, COVID-19 hospitalizations are at levels not seen since February.
But there are signs now that this summer wave may have now reached its peak across some states in this region, where the virus first picked up steam.
Forecasts updated by the CDC this week estimate that COVID-19 infections are growing across almost all states, but are “stable or uncertain” in three: Hawaii, Oregon and New Mexico.
“It’s hard to predict the future. And if COVID has taught is anything, it’s that things can always change. But based on previous trends, where we have seen sort of a summer wave that has peaked around July or August, is what we might expect for this year,” said Hall.
Nursing home infections have slowed for a second straight week in the Pacific Northwest, in the region spanning Alaska through Oregon.
In Hawaii, where COVID-19 emergency room trends this summer had peaked at levels worse than both their last winter and summer waves of the virus, patients have slowed for multiple weeks now.
Hall cautioned that while COVID-19 trends have slowed after summer peaks in recent years, they still remained far worse than the low levels seen during past springtime lulls in the virus.
“We don’t see necessarily a nadir or bottoming out, between the summer and winter waves, at least historically. So that’s important as we think about protecting people that are vulnerable,” he said.
What is the latest variant in this COVID-19 wave?
The CDC last updated its every-other-week variant projections after the Fourth of July, estimating that the KP.3 variant had grown to more than a third of infections nationwide.
Behind it were the KP.2 and LB.1 variants, two close relatives that are all descendants of the JN.1 strain that dominated infections this past winter. Put together, these three variants — KP.3, KP.2 and LB.1 — made up more than 3 in 4 infections nationwide.
Hall said there is “still no indication of increased severity of illness” associated with any of these variants, similar to what the agency has said in recent weeks.
Hall said the agency tracks data from hospitals and ongoing studies, as well as detailed analyses of the genetic changes to the virus, to search for signs that the risk from new variants might have grown.
“None of those data sources have given us any indication that these variants cause more severe disease than what we have seen previously,” he said.
Through the end of June, the CDC estimated that all regions of the country were seeing a mix of these strains, though some more than others depending on the location.
KP.3 makes up the largest share of infections in several regions of the country, while LB.1 is larger around the New York and New Jersey area and KP.2 is bigger in New England.
For now, Hall said KP.3 and LB.1 are the variants that are spreading fastest, though their relative growth looks to be “considerably lower” than previous highly mutated strains like the original Omicron variant.
“It’s not anything as dramatic as some of the earlier shifts in the virus that we’ve seen,” he said.
FALL VACCINE UPDATE

The following is the recommendation from the CDC on fall vaccines. It covers flu, Covid as well as new recommendations for who should get the RSV vaccine.
CDC Recommends Updated 2024-2025 COVID-19 and Flu Vaccines for Fall/Winter Virus Season
For Immediate Release: June 27, 2024
Contact: Media Relations
(404) 639-3286
Today, CDC recommended the updated 2024-2025 COVID-19 vaccines and the updated 2024-2025 flu vaccines to protect against severe COVID-19 and flu this fall and winter.
It is safe to receive COVID-19 and flu vaccines at the same visit. Data continue to show the importance of vaccination to protect against severe outcomes of COVID-19 and flu, including hospitalization and death. In 2023, more than 916,300 people were hospitalized due to COVID-19 and more than 75,500 people died from COVID-19. During the 2023-2024 flu season, more than 44,900 people are estimated to have died from flu complications.
Updated 2024-2025 COVID-19 Vaccine Recommendation
CDC recommends everyone ages 6 months and older receive an updated 2024-2025 COVID-19 vaccine to protect against the potentially serious outcomes of COVID-19 this fall and winter whether or not they have ever previously been vaccinated with a COVID-19 vaccine. Updated COVID-19 vaccines will be available from Moderna, Novavax, and Pfizer later this year. This recommendation will take effect as soon as the new vaccines are available.
The virus that causes COVID-19, SARS-CoV-2, is always changing and protection from COVID-19 vaccines declines over time. Receiving an updated 2024-2025 COVID-19 vaccine can restore and enhance protection against the virus variants currently responsible for most infections and hospitalizations in the United States. COVID-19 vaccination also reduces the chance of suffering the effects of Long COVID, which can develop during or following acute infection and last for an extended duration.
Last season, people who received a 2023-2024 COVID-19 vaccine saw greater protection against illness and hospitalization than those who did not receive a 2023-2024 vaccine. To date, hundreds of millions of people have safely received a COVID-19 vaccine under the most intense vaccine safety monitoring in United States history.
Updated 2024-2025 Flu Vaccine Recommendation
CDC recommends everyone 6 months of age and older, with rare exceptions, receive an updated 2024-2025 flu vaccine to reduce the risk of influenza and its potentially serious complications this fall and winter. CDC encourages providers to begin their influenza vaccination planning efforts now and to vaccinate patients as indicated once 2024-2025 influenza vaccines become available.
Most people need only one dose of the flu vaccine each season. While CDC recommends flu vaccination as long as influenza viruses are circulating, September and October remain the best times for most people to get vaccinated. Flu vaccination in July and August is not recommended for most people, but there are several considerations regarding vaccination during those months for specific groups:
- Pregnant people who are in their third trimester can get a flu vaccine in July or August to protect their babies from flu after birth, when they are too young to get vaccinated.
- Children who need two doses of the flu vaccine should get their first dose of vaccine as soon as it becomes available. The second dose should be given at least four weeks after the first.
- Vaccination in July or August can be considered for children who have health care visits during those months if there might not be another opportunity to vaccinate them.
- For adults (especially those 65 years old and older) and pregnant people in the first and second trimester, vaccination in July and August should be avoided unless it won’t be possible to vaccinate in September or October.
Updated 2024-2025 flu vaccines will all be trivalent and will protect against an H1N1, H3N2 and a B/Victoria lineage virus. The composition of this season’s vaccine compared to last has been updated with a new influenza A(H3N2) virus.
For more information on updated COVID-19 vaccines visit: Coronavirus Disease 2019 (COVID-19) | CDC. For more information on updated flu vaccines visit: Seasonal Flu Vaccines | CDC.
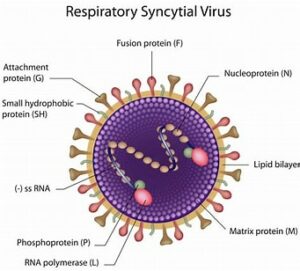
Simpler recommendations on RSV vaccines for older adults
ACIP offered clearer guidance around the use of the respiratory syncytial virus (RSV) vaccines for older adults. RSV vaccines for older adults became available for the first time in the United States last year.
Older adults are at higher risk of developing severe RSV. The initial recommendations called for adults 60 years and older to receive one dose of the RSV vaccine based on shared clinical decision making, that is, a conversation between patient and healthcare provider about whether the shot was appropriate for them based on their health conditions. In the context of new data that are now available on RSV vaccines for older adults, the recommendations were updated to be more specific and streamlined.
The updated RSV vaccine recommendations for adults 60 years and older are age- and risk-based. ACIP now recommends all adults 75 years of age and older receive a single dose of RSV vaccine. Adults 60 to 74 years of age should get a single dose of RSV vaccine if they are at increased risk of severe RSV disease. Adults ages 60 to 74 are at higher risk if they have certain chronic medical conditions, such as lung or heart disease, or if they live in a nursing home or long-term care facility.
RSV vaccination is currently recommended as a one-time dose. If you have already received RSV vaccination, another dose is not recommended for you at this time.
RSV immunization recommendations to protect infants, either through maternal vaccination or RSV antibody given to the baby after birth, stayed the same. CDC continues to recommend RSV immunizations to protect all babies from severe RSV.

FLU VACCINE:
We will start giving flu vaccinations after Labor Day. The optimal time to get on is in September to October. I try to get mine in October. If one gets it too early there is the concern that antibodies will drop by the time the flu rolls around in the winter months. Often, people want to get it right away. That’s not necessary. If you have an appointment this fall you can get it, then. We do like schedule appointments for these. As in previous years if you wear a short-sleeved shirt you can remain in your car and one of our staff will come out and give it to you.
MEDICARE DISADVANTAGE
About 50% of Medicare patients are Medicare replacement policies, also known as Medicare Advantage plans. They offer additional perks like eyeglasses and gym memberships. They also offer easy of billing. They are a good deal until they are not. If you need to have a procedure or an MRI, they have to give authorization which can cause delays. Also, they are often asking us for additional information about their subscribers which they are legally entitled to do. As outlined in a recent Wall Street Journal article (How the Journal Analyzed Medicare Advantage Data – WSJ ) they do this so that they can charge the government more money. Another thing they do is to send nurses out for an exam, not to check on you, but to gather more diagnoses to justify higher payment. Let the buyer beware.
Wishing you the best of health.
Mark L. Thornton, M.D., F.A.C.P.